
A DIGITAL HEALTH PLAYBOOK
How Digital Health Will Decide the Winners in the $10B MASH Market
PLEASE ENJOY YOUR EXCERPT OF OUR PLAYBOOK BELOW
Chapter 1: Why Digital Whole-Person Care is Now Mission-Critical
-
Whole-person digital health is the integration of digital tools and care pathways that address not just a disease, but the full spectrum of a patient’s physical, mental, behavioral, and social needs.
-
For MASH, whole-person digital health means pairing breakthrough therapies with digital solutions that support weight, cardiometabolic risks, mental health, lifestyle, and adherence—delivering care that goes beyond the pill.

MASLD affects ~1 in 3 U.S. adults, with ~16M progressing to MASH. A wave of nine therapies (beginning 2024) won’t succeed as medicines alone. Because MASH travels with obesity, diabetes, hypertension, and mental-health burden, outcomes demand a whole-person approach. This chapter shows why digital health—screening, engagement, mental health, coaching, cardiometabolic support, and adherence—must be the operating system that turns FDA drug approvals into whole-person, real-world impact.
MASLD: The “Silent Epidemic” Touching ~1 in 3 U.S. Adults
Metabolic dysfunction–associated steatotic liver disease (MASLD, formerly NAFLD) now affects roughly a third of U.S. adults. Recent decision-analytic modeling estimates 33.7% (≈86 million) of adults had MASLD in 2020, rising further by 2050; MASH (the progressive inflammatory form) affected ~14.9 million in 2020, trending toward 18–23 million by 2030–2050. Our estimates, shown in Exhibit 1.1, suggest that nearly 42% of U.S. adults will have MASLD by 2050.
Exhibit 1.1: MASLD Prevalence in the U.S.

NHANES (National Health and Nutrition Examination Survey) elastography analyses and recent guidance pieces align on a ~25–30% adult prevalence range today, with ~11% showing clinically relevant fibrosis on vibration-controlled elastography—typically asymptomatic until advanced.
For context, type 2 diabetes affects ~11–12% of U.S. adults, making MASLD ≈2–3× larger, yet far less recognized—hence “silent.” Exhibit 1.2 compares the prevalence of MASH and MASLD to other common cardiometabolic medical conditions, revealing the surprising high prevalence versus T2D, obesity, and hypertension.
Exhibit 1.2: Prevalence of Cardiometabolic Conditions in the U.S.

Implication: Even modest improvements in education and awareness among patients and clinicians can meaningfully increase detection and management for this large population.
A Therapeutic Wave: 2024 Kicked Off the MASH Rx Era
In 2024 the FDA approved the first MASH therapy that enabled Madrigal Pharmaceuticals to bring its Rezdiffra (resmetirom) to market to treat patients with moderate-to-advanced fibrosis (MASH F2/F3) – to be used with diet and exercise. This latter indication is an area where our traditional health system has failed to engage patients to change important lifestyle behaviors to improve their overall health condition, and this will require pharmaceutical companies to adopt more innovative whole-person digital health solutions to move the needle on many of the comorbid symptoms of MASH.
In the following year, 2025, the FDA granted accelerated approval to semaglutide (Wegovy, developed and commercialized by Novo Nordisk) for MASH with moderate-to-advance fibrosis (non-cirrhotic), becoming the second approved therapy and the first GLP-1 for this indication.
Exhibit 1.3: Expected Timeline of MASH Rx Commercial Launches
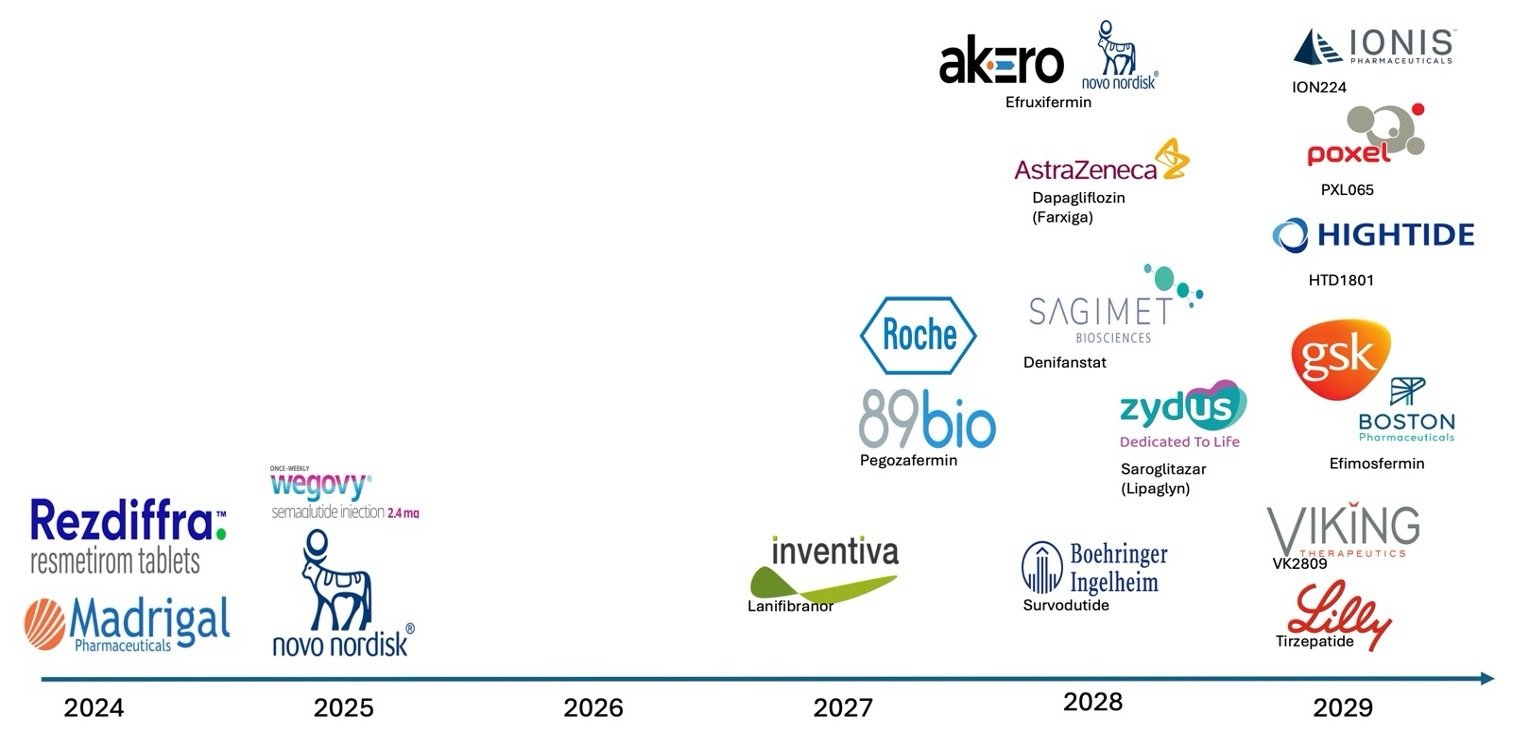
Beyond these, a late-stage pipeline of more than 9 assets, which spans distinct mechanisms (FGF21 analogs efruxifermin, pegozafermin; pan-PPAR lanifibranor; THR-β agonists; FASN inhibitors; incretin-based combinations), have advanced through multiple Phase 2/3 readouts since 2024, with FDA filings expected through the second half of the decade.
Implication: Drug innovation is accelerating—but medicines alone won’t address behavioral, cardiometabolic, and psychosocial drivers that determine real-world outcomes. A whole-person digital health solution that goes beyond-the-pill and that leverage multiple technologies along the entire patient journey and comorbid symptoms must be offered to patients to move the needle.
MASH is Multisystemic: Heavy Cardiometabolic and Mental Health Comorbidities
Comorbidity analysis shown in Exhibit 1.4 makes it clear that MASLD/MASH patients travel with high levels of comorbidities among cardiometabolic and mental health conditions. Among patients with obesity, nearly a third have MASH, while 70% of severely obese patients have MASH, and among MASH patients, over 80% have obesity. Among patients with T2D, nearly 40% have MASH, and among MASH patients about 45% have T2D. Patients with hypertension have a much lower comorbidity with MASH at about 15%, but among MASH patients, nearly 70% have hypertension; cardiovascular disease is a major cause of morbidity and mortality in this population, prompting guideline calls for aggressive risk-factor management.
Exhibit 1.4: MASH Comorbidities

MASH patients suffer from substantial psychological burden: pooled estimates show depression ~26% and anxiety ~37% in MASLD, with several cohorts reporting over a third of patients meeting anxiety/depression thresholds and higher risk over time, with higher levels as disease severity increases.
Implication: Optimal MASH care must be whole-person—combining liver-directed therapy with cardiometabolic control, mental-health support, nutrition, activity, sleep, and social determinants of health.
Digital Health is The Operating System for Whole-Person MASH Care
Whole-person digital health is the integrated use of digital technologies to support the full spectrum of a patient’s physical, mental, emotional, behavioral, and social needs across the care continuum. Rather than focusing narrowly on a single condition or intervention, whole-person digital health solutions combine evidence-based digital tools—such as remote monitoring, mobile health self-care therapeutic and wellness applications, telehealth, virtual coaching, behavioral health platforms, and connected devices—this enables personalized care pathways that address comorbidities, lifestyle factors, and psychosocial determinants of health.
Key characteristics for whole-person digital health solutions include:
Holistic scope: Encompasses not only disease-specific management (e.g., MASH treatment) but also the interconnected domains of cardiometabolic risk, mental health, lifestyle behaviors, and social well-being.
Integration with traditional care: Bridges digital interventions with pharmacotherapy, clinician oversight, and health-system infrastructure, ensuring seamless patient experiences and provider workflows.
Personalization and adaptivity: Leverages patient-reported outcomes, biometrics, and behavioral data to deliver tailored interventions that adapt to an individual’s preferences and needs over time.
Scalability and accessibility: Uses digital platforms to expand access to care, reduce disparities, and provide continuous, low-friction support beyond the clinic.
In the context of MASH, whole-person digital health means not only delivering medications that target liver pathology but also addressing the weight management, diabetes, cardiovascular risk, depression, anxiety, sleep, and lifestyle factors that drive disease progression and outcomes.
Such a comprehensive whole-person digital platforms enable identification, triage, engagement, and longitudinal support at scale—exactly what MASH care requires:
- Screening & risk stratification: Integrated e-PROs, EHR algorithms, and home diagnostics can surface at-risk patients (e.g., T2D/obesity cohorts) and route to non-invasive testing—reducing reliance on invasive diagnostics and late referrals. (Aligned to AASLD/AACE guidance emphasizing risk-factor management and non-invasive pathways.)
- Lifestyle & behavior change: Digital health and remotely delivered programs in fatty-liver populations show feasibility, weight loss, improved liver enzymes, and behavior change, providing a scalable adjunct to pharmacotherapy.
- Integrated chronic-care management: Telehealth/remote monitoring frameworks have proven value across chronic diseases and are endorsed in global strategies (WHO) for health-system strengthening—relevant for multi-comorbidity MASH.
The following Exhibit 1.5 describes each of the five dimensions of Whole-Person Health as it applies to MASH patients and the role of different type of both clinical and non-clinical care providers and other stakeholders in delivering each part the experience. It also describes the different types of digital health products and services that align with each of the five Whole-Person digital health experience.
Exhibit 1.5: Whole-person Digital Health Features and Benefits

Implication: To translate approvals into outcomes, pharma must pair MASH medicines with digital whole-person programs (cardiometabolic risk control, mental-health support, nutrition/activity coaching, adherence, and navigation), integrated into HCP workflows, DTC engagement programs, and community settings.
